Chronic Condition Management Plan (CCMP) changes
Learn about how the changes from CDM items to CCMP items may impact your Practice and gain practical insights into managing these changes.
The Australian Government will be ceasing Chronic Disease Management (CDM) items and introducing new, streamlined Chronic Condition Management Plan (CCMP) items from 1st July 2025. These metrics are designed to help you understand the changes, how they may impact your practice, and provide tools to manage the transition.
This feature is available to our Best Practice software integration customers.
Cubiko's dashboard analyses historical services and billings for the ceasing CDM items, to highlight the possible impact of the new CCM items if delivered at the same rate of care and using the new rebate amounts.
NOTE: Please note that this data is provided purely for financial analysis and is not intended to be used as a claiming guideline.
- Where Practitioners were previously able to bill for multiple eligible services related to Chronic Disease Management plans and reviews on a single invoice for a single patient, from 1st July, these items will cease and be replaced with new streamlined items for care planning.
- Under the new changes, only one item 965 or 967 can be provided per day.
- The new items from 1st July 2025 are Chronic Condition Management Plans (CCMP).
-
Previously, items 721 and 723 could be provided consecutively, and their respective reviews could be conducted similarly. However, this will no longer be possible with the new CCMP plans.
These calculations only consider same-day services. For patients billed with items 721 and 723 within 12 months: if these were billed on the same day, they count as a single 965 item; if billed on different days, they count as two 965 items. Similar for reviews.
In this metric CDM items are 721, 723, 732, 229, 290, 233, 92024, 92025, 92028, 92055, 92056 and 92059. We do not include Health assessments or nursing items in these calculations.
To navigate to this metric, go to the Industry Updates tab > Chronic Condition Management Plans

Download the Chronic Condition Management (CCM) dashboard here.
The sections included in this article are:
- Understanding the Changes
- What Is the GP Chronic Condition Management Plan?
- What Happens to Existing GPMP and TCA Patients?
- Timeline of changes
- Key MBS Item Changes
- Will These Changes Affect Practice Revenue?
- How Does MyMedicare Fit Into This?
- How Cubiko can help you transition
- Impact and insights tab
- Key metrics to see the impact of the changes, and make informed decisions
- Operational support tab
- Key metrics relating to My Medicare registrations
- Resources tab
- Impact and insights tab
-
Other key metrics in Cubiko to help you support this transition
- Additional resources and tools
Understanding the Changes
In 2022, the Strengthening Medicare Taskforce was established with the goal of improving patient access, affordability, and management of ongoing and chronic conditions. As part of this initiative, major changes to the Medicare Benefits Schedule (MBS) will take effect from 1st July 2025.
The biggest shift: Item numbers 721, 723, and 732 will be removed. These will be replaced by new items under the GP Chronic Condition Management Plan (GPCCMP) framework.
What Is the GP Chronic Condition Management Plan?
The GP Chronic Condition Management Plan (GPCCMP) is a new, streamlined way to manage patients with chronic conditions. These plans are designed to:
-
Simplify care coordination
-
Support multidisciplinary team involvement
-
Ensure more consistent patient outcomes
The current GP Management Plans (GPMPs) and Team Care Arrangements (TCAs) will be phased out and replaced with new item numbers that combine elements of both care models.
What Happens to Existing GPMP and TCA Patients?
Good news:
Patients with an existing GPMP or TCA in place before 1st July 2025 will continue to be able to access care under that plan for two years. These plans will not need to be redone or converted.
However, any new care plans initiated from 1st July 2025 onwards must use the new GPCCMP item numbers. To be able to bill a CCMP review (967), a patient must have been billed a GPCCMP (965) at least 3 months prior.
Timeline of changes
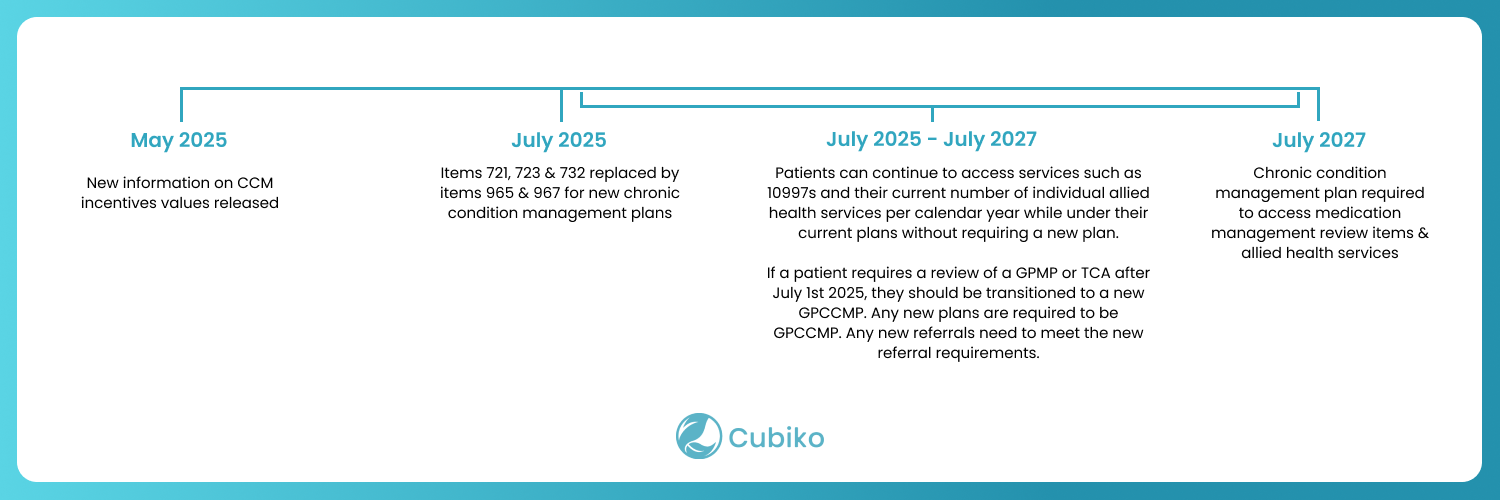
TOP TIP: Visit trusted sources for further information to better understand the changes: Additional resources
Key MBS Item Changes
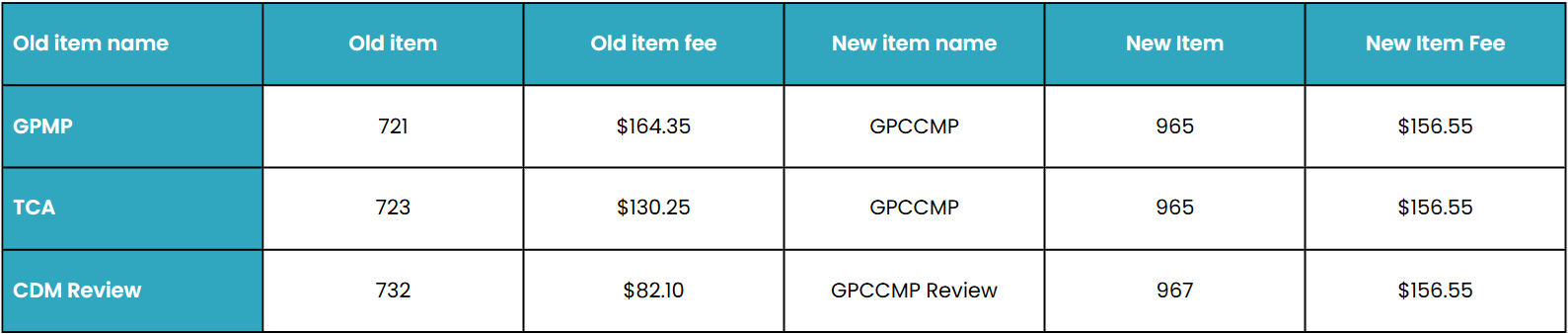
⚠️ Important: From 1st July 2025, only one CCMP item (965 or 967) can be billed per day. Unlike before, you can no longer bill a 721 and a 723 together on the same day.
The same applies to reviews - From 1st July, there is only one plan to review, whereas previously, both could be reviewed and billed.
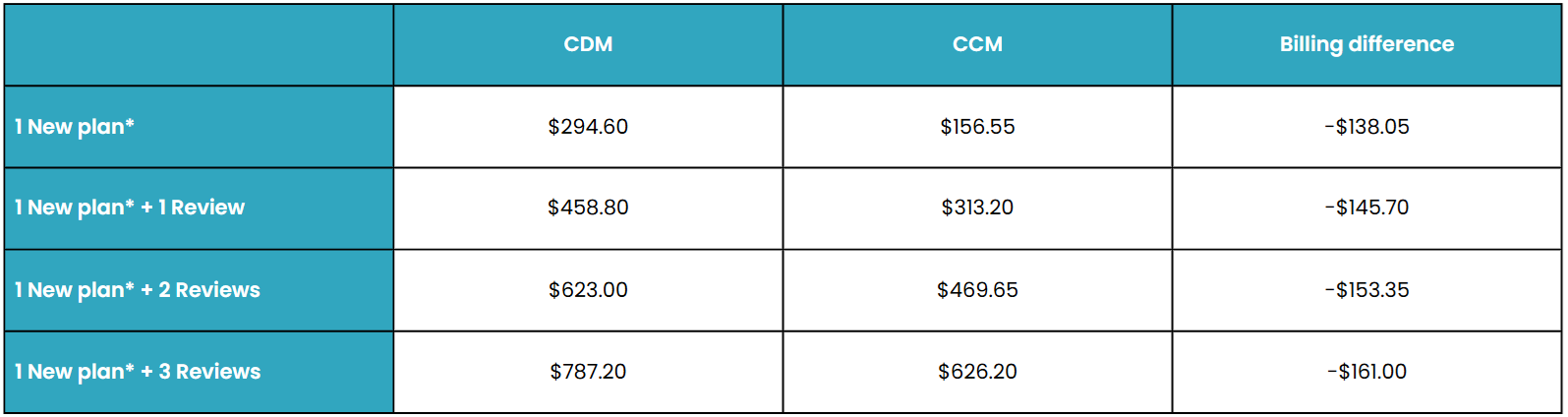
Will These Changes Affect Practice Revenue?
Yes - and how much depends on your review frequency.
Here’s what we’ve learned from conference discussions and early modelling:
-
Previously, GPMP + TCA (721 + 723) billed together = more revenue.
-
Now, only one item (965) is billable for plan development.
-
Revenue drops if no extra reviews are conducted.
-
More frequent reviews (every 3 months) could offset or exceed the reduction, but this may not be practical in every setting.
Example:
12 months of billing, existing bulk billing incentives.
How Does MyMedicare Fit Into This?
-
Patients registered via MyMedicare can only receive a CCMP through their nominated practice - this reinforces continuity of care.
- Having patients registered to your practice reduces the ability for other practices to bill a patient for a care plan, where they are not a usual patient.
-
Non-registered patients can continue receiving care through their usual GP as before.
How Cubiko Can Help You Transition
We have developed new metrics and dashboards to assist your practice in navigating the transition seamlessly. Cubiko's metrics evaluate historical services and billings for the discontinued CDM items to illustrate the potential impact of the new CCM items if provided at the same level of care and utilising the updated rebate amounts.
Impact and insights tab
Financial impact of CDM changes
Cubiko’s dashboard analyses historical services and billings for the ceasing CDM items, to highlight the possible impact of the new CCMP items and their new value, if delivered at the same rate of care.
The items Cubiko is classifying as CDM include: 721, 723, 732 and their equivalents. We do not include Health assessments or nursing items in these calculations. Please note that this section is purely for financial analysis and is not intended to be used as a claiming guideline.
| Metric | Description |
|---|---|
|
Change to CDM revenue
|
In the selected time period, this metric shows the difference in historical CDM billings if new CCMP rebates and rules were applied. It reflects changes where both 721 and 723 were billed, now only item 965 can be claimed. It also includes the loss of bulk billing incentives, as only one incentive can be claimed instead of two. Do you need to review any processes or workflows in the practice to compensate for any losses? Such as being more proactive in the Health Assessment space? Or are you expecting the eligible patient cohort to expand with the new rules and have planned accordingly? |
|
CDM % of total billings
|
This metric shows the proportion of billings for Chronic Disease Management at your practice in the time frame selected. This is based upon the existing services billed for GPMP/TCA/Reviews. Are you expecting your CDM/CCMP rate to stay the same, increase, decrease? What level of change is tolerable? |
|
Patients with CDM in 12 months
|
This metric displays the total number of patients who received CDM billings in the past 12 months, broken down by those who were billed for single CDM item versus those who had multiple CDM items on one day. This is useful to see how frequently your patients are currently having their care plans reviewed either alone, or together. Have you historically billed your GPMP and TCA together? And both the reviews? How will this impact your practice? |
CDM billings by Practitioner |
This figure represents chronic disease management (CDM) billings (inclusive of GST, and based on service date) per Practitioner. |
Reviews per patient |
This shows how often patients are being reviewed. It counts how many eligible patients had: 1 review, 2 reviews, and so on — over the past 12 months. This helps you see how regularly patients are being followed up and how engaged they are in their care. |
Breakdown of CDM service equivalents
Under the new changes, only one item 965 or 967 can be provided per day. Previously, items 721 and 723 could be provided consecutively and their respective reviews could be conducted similarly. However, this will no longer be possible with the new CCMP plans.
These calculations only consider same-day services. For patients billed with items 721 and 723 within 12 months: if these were billed on the same day, they count as a single 965 item; if billed on different days, they count as two 965 items. Similar for reviews.
| Metric | Description |
|---|---|
|
New Item 965 equivalents (care plans) rebate under the CCMP changes
|
Under the new changes, TCA (723) and GPMP (721) will be replaced by one single item – 965. |
|
New Item 967 equivalents (reviews) rebate under the CCMP changes
|
This shows a comparison between past review billing and what it would look like under the new CCMP system. |
|
Lost bulk billing incentives under the CCMP changes
|
With the new CCMP item replacing both the TCA (723) and GPMP (721), you’ll only be able to charge one bulk billing incentive instead of two. |
CDM related opportunities
Outside of the immediate financial implications, the removal of administrative overhead and the new billing structure may allow for more streamlined care delivery. This section provides insights into potential areas of focus to provide the best quality care and to make the most of your existing resources. Review the following metrics to identify potential new patients who may benefit from a care plan, to understand the current unserviced CDM eligible patient population, and to consider how to best utilise the practices nurse time.
| Metric | Description |
|---|---|
Fulfilment of CDM opportunity by Doctor
|
Fulfilment of CDM opportunity by DoctorThis graph shows how well each doctor is making the most of CDM opportunities. |
|
Potential new CDM patients
|
This metric shows how many patients with a chronic or ongoing condition have: |
|
Nurse consulting utilisation
|
This shows how much of a nurse’s available time is being used to see patients. It’s calculated by comparing:
This helps you understand how effectively nurse time is being used and spot opportunities to improve scheduling or patient flow. |
Details
This table shows how much you would have earned using the new CCMP items, compared to your previous CDM billing.
-
Past 721 and 723 items are shown as ‘Item 965 equivalents’
-
Past 732 items are shown as ‘Item 967 equivalents’
It’s a quick way to see how the new rebates compare to your previous billing totals under the old system.

Filters

Top Tips for Using Filters to Get the Best Data Outcome
-
Set Dates to cover the period you want to analyse (e.g., 1 May 2025 to 31 May 2025)
-
Choose Practitioner Role (e.g., GP) and select a specific practitioner to focus on their patients and performance
-
Filter by Usual Doctor to see patients mainly managed by that practitioner
-
Optionally filter by MyMedicare registered patients to focus on patients eligible for CCMP and rebates
-
Turn on Exclude unpaid services to only include completed, paid appointments for accurate billing and rebate data
-
Use these filters to:
-
Track lost bulk billing incentives under CCMP changes
-
Forecast rebates for new CCMP items compared to old billing
-
Measure CDM opportunity fulfilment per doctor
-
Identify patients without a current care plan
-
Review nurse consulting utilisation if applicable
-
Compare total rebate amounts between old and new billing items
-
This approach helps you get clear insights on practitioner performance, patient care opportunities, and financial impact under the new CCMP system.
Operational support tab
MyMedicare Requirements
Patients enrolled in MyMedicare can only receive CCM services at the practice where they are registered.
If a patient is not enrolled in MyMedicare, they can still get CCM items from their usual doctor at any practice.
To avoid any issues, it’s best to encourage patients to register both with your practice and with the doctor who will be providing their care. This helps make sure they stay eligible for the services and rebates.

-
Click on the “Percentage of CDM patients who are MyMedicare registered”
-
This shows you what portion of your eligible CDM patients are registered with MyMedicare.
-
Use this to identify how well your practice is capturing registrations and to find opportunities to encourage more patients to register.
-
-
Check “MyMedicare eligible patients with an appointment today”
-
This tells you which patients who qualify for MyMedicare have an upcoming appointment.
-
Use this list to remind or assist patients with registering during their visit, since registration usually requires two face-to-face visits within two years.
-
Resources tab
See additional resources here: bottom of page

Other key metrics in Cubiko to help you support this transition
TOP TIP: Complete these before 1st July 2025!
The following MBS items are being removed: 721, 723, and 732. To get the most value out of existing care plans, review and action all outstanding actions related to these items before this date.
| Metric | Action |
| Item Optimisation – 721, 723 | Review all eligible patients and ensure item numbers 721 and 723 are claimed before 1st July 2025 |
| Item Optimisation – 732 (x2) | Ensure both eligible 732 items are claimed for patients before they are removed from MBS on 1st July 2025. |
| Uncompleted and Unbilled Appointments | Review all care plan appointment types (including reviews). Check that the relevant item numbers (721, 723, 732) have been billed. Follow up on any unbilled appointments and complete billing prior to the cut-off date. |
| Billings on Hold | Check for 721, 723, or 732 items currently on hold (e.g. waiting on signed TCAs). Use this time to follow up and finalise billing before the items are no longer claimable after 1st July 2025. |
| Outstanding Debt | Filter the billing list by item number (721, 723, 732) and review the "MBS item" column. If any items were billed to Patient instead of Medicare, correct and resubmit the claim before 1st July 2025. |
| Outstanding Rejections | Check for any 721, 723, or 732 rejections in your billing system. Take steps to resolve and resubmit these claims before the items are removed from the MBS |
Final Checklist Before 1st July 2025
✅ Finalise and bill 721, 723, and 732 items
✅ Complete unbilled and uncompleted care plan appointments
✅ Resolve billings on hold, debtors, and rejections for CDM items
✅ Flag new patients using CCMP eligibility metrics
✅ Educate your team on the new items use
TOP TIP: Download and share the Chronic Condition Management Resource Pack with your team to help them better understand the changes.
Additional resources and tools
-
Visit MBS Online for official resources:
-
Cubiko Blog: Everything practices need to know about the new Chronic Condition Management Announcements
- Downloadable resource: Chronic Condition Management Resource Pack









